Leads on ECG: 12 Essential Facts You Must Know Now
Ever wondered how a simple 12-lead ECG can reveal the secrets of your heart? It’s not just lines on paper—it’s a powerful diagnostic tool that doctors rely on every day.
What Are Leads on ECG and Why They Matter

The term leads on ecg refers to the electrical perspectives of the heart recorded by electrodes placed on the body. These leads provide clinicians with a multidimensional view of cardiac activity, allowing them to detect abnormalities in rhythm, conduction, and even structural damage.
Understanding the Basic Concept of ECG Leads
An electrocardiogram (ECG or EKG) measures the heart’s electrical activity over time. Each lead represents a specific angle from which this activity is viewed. Think of it like taking photos of the heart from different directions to get a complete picture.
- There are 12 standard leads in a routine ECG.
- Each lead captures voltage differences between electrodes.
- The leads are grouped into limb and precordial categories.
These leads do not measure individual electrical impulses but rather the overall direction and magnitude of the heart’s depolarization wavefront.
The Role of Leads in Clinical Diagnosis
Accurate interpretation of leads on ecg is crucial for diagnosing conditions such as myocardial infarction, arrhythmias, and electrolyte imbalances. For example, ST-segment elevation in certain leads can pinpoint the location of a heart attack.
“The 12-lead ECG is one of the most widely used tools in cardiology because it’s non-invasive, quick, and highly informative.” — American Heart Association
Doctors use patterns across multiple leads to differentiate between anterior, inferior, lateral, and posterior wall involvement during acute coronary syndromes.
Types of Leads on ECG: Limb vs Precordial
The 12 leads on a standard ECG are divided into two main groups: the six limb leads and the six precordial (chest) leads. Each group provides unique insights into the heart’s function.
Limb Leads: Capturing Vertical Plane Activity
The limb leads—comprising three standard limb leads (I, II, III) and three augmented limb leads (aVR, aVL, aVF)—record electrical activity in the frontal plane. This means they look at the heart from top to bottom and side to side.
- Lead I measures the voltage difference between the right and left arms.
- Lead II is often used for rhythm monitoring due to its clear P wave visibility.
- aVR is unique because it looks at the heart from the right shoulder and is often ignored—but shouldn’t be.
These leads help identify axis deviations, inferior wall MI, and limb lead reversals. You can learn more about their clinical significance at American Heart Association.
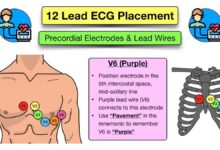
Precordial Leads: Mapping Horizontal Plane Signals
The precordial leads (V1 to V6) are placed across the chest and record electrical activity in the horizontal plane. They are essential for detecting anterior, septal, and lateral wall changes.
- V1 and V2 face the septum and right ventricle.
- V3 and V4 reflect the anterior wall of the left ventricle.
- V5 and V6 monitor the lateral wall.
Because these leads are unipolar, they measure the voltage at one point relative to a central terminal. Their positioning must be precise; even small shifts can alter readings significantly.
How ECG Leads Are Placed: Step-by-Step Guide
Proper electrode placement is critical to ensure accurate leads on ecg. Misplacement can lead to misdiagnosis, including false positives for myocardial infarction.
Standard Limb Lead Placement
Limb leads are attached to the arms and legs, though in practice, they are usually placed on the wrists and ankles to minimize movement artifacts.
- RA (Right Arm): Inner wrist or upper arm.
- LA (Left Arm): Same as RA on the left side.
- RL (Right Leg): Ankle or lower abdomen (ground electrode).
- LL (Left Leg): Opposite leg, ensuring symmetry.
It’s important that the electrodes are not placed directly over muscle masses to avoid interference from skeletal muscle activity.
Precordial Lead Placement: The Chest Grid
The chest leads follow a specific anatomical roadmap:
- V1: 4th intercostal space, right sternal border.
- V2: 4th intercostal space, left sternal border.
- V3: Midway between V2 and V4.
- V4: 5th intercostal space, midclavicular line.
- V5: Anterior axillary line, same horizontal level as V4.
- V6: Midaxillary line, same level as V4 and V5.
Incorrect placement of V1 and V2 too high can mimic anterior MI, while misplaced V4–V6 can distort lateral wall readings. For detailed placement guidelines, visit ECG Waves.
“A misplaced V1 electrode can mimic Brugada pattern or right bundle branch block—leading to unnecessary interventions.”
The Electrical Axis and Its Relationship to Leads on ECG
The QRS axis represents the overall direction of ventricular depolarization. It is determined primarily by analyzing the limb leads, especially I, II, and III.
What Is the Normal QRS Axis?
The normal QRS axis ranges from -30° to +90°. This means the main vector of depolarization points downward and to the left, reflecting the dominance of the left ventricle.
- Positive deflection in leads I and II indicates normal axis.
- Negative in I and positive in II suggests right axis deviation.
- Positive in I and negative in II may indicate left axis deviation.
Axis determination helps localize conduction blocks and structural heart disease.
How Leads on ECG Help Determine Axis Deviation
By examining the net QRS deflection in leads I and aVF, clinicians can estimate the electrical axis using the quadrant method.
- Right Axis Deviation (>+90°): Seen in right ventricular hypertrophy, pulmonary embolism, or chronic lung disease.
- Left Axis Deviation (<-30°): Associated with left anterior fascicular block or inferior MI.
- Extreme Axis Deviation (-90° to ±180°): Rare and often indicates serious conduction issues.
For example, a deep S wave in lead I and tall R wave in lead III suggest right axis deviation, commonly seen in patients with COPD.
Interpreting ST Changes Across Leads on ECG
One of the most critical applications of leads on ecg is identifying ST-segment changes, which are key indicators of myocardial ischemia or infarction.
ST Elevation: Location-Specific Patterns
ST elevation in specific leads corresponds to the area of the heart affected:
- II, III, aVF: Inferior wall MI.
- V1–V4: Anterior wall MI.
- I, aVL, V5–V6: Lateral wall MI.
- V1–V3 with right-sided leads (V4R): Right ventricular MI.
It’s vital to correlate ST changes with clinical symptoms and cardiac biomarkers. Not all ST elevation indicates infarction—conditions like pericarditis or early repolarization must be ruled out.
“In acute STEMI, time is muscle. Rapid interpretation of leads on ecg can save lives.”
For more on ST elevation patterns, refer to Life in the Fast Lane ECG Library.
ST Depression and Its Clinical Implications
ST depression often indicates subendocardial ischemia and can be horizontal or downsloping.
- Widespread ST depression with ST elevation in aVR suggests global ischemia, possibly from left main coronary artery disease.
- Reciprocal ST depression in leads opposite an MI (e.g., ST depression in aVL during inferior MI) supports the diagnosis.
- Strain patterns in left ventricular hypertrophy also show ST depression with asymmetric T wave inversion.
However, digitalis effect can cause scooped ST depression without pathology, so clinical context is essential.
Common Errors in Reading Leads on ECG
Even experienced clinicians can misinterpret leads on ecg due to technical errors, lead misplacement, or pattern recognition mistakes.
Lead Reversal: A Frequent Pitfall
Arm lead reversal (LA-RA swap) is one of the most common errors. It causes:
- Inverted P waves, QRS complexes, and T waves in lead I.
- Lead II and III become swapped.
- aVR and aVL also switch roles.
This can mimic dextrocardia or atrial abnormalities. Clues include a positive P wave in aVR and a negative QRS in lead I.
Incorrect Chest Lead Placement
Placing V1 and V2 too high (e.g., 2nd or 3rd intercostal space) can create a Brugada-like pattern. Similarly, placing V3–V6 too high or too lateral distorts the transition zone.
- Misplaced V leads can mimic anterior MI or mask real changes.
- Failure to place V4 at the 5th ICS midclavicular line alters sensitivity for anterior infarcts.
- Using the wrong intercostal space affects R wave progression.
A study published in the Journal of Electrocardiology found that up to 40% of ECGs have some degree of lead misplacement.
Advanced Applications of Leads on ECG
Beyond the standard 12-lead ECG, advanced techniques use additional leads to enhance diagnostic accuracy, especially in complex cases.
Right-Sided ECG Leads (V4R to V6R)
When suspecting right ventricular infarction (often accompanying inferior MI), right-sided leads are placed:
- V4R: 5th ICS, midclavicular line on the right side.
- V5R and V6R: Continue laterally.
ST elevation in V4R is highly sensitive for right ventricular involvement and guides fluid management and thrombolytic therapy.
“Don’t forget the right side—RV infarction can be silent on a standard 12-lead.”
For more on right-sided ECGs, see NCBI Article on Right-Sided ECG.
Posterior Leads (V7–V9)
Posterior MI is often missed because standard leads don’t cover the back wall. Posterior leads are placed:
- V7: Left posterior axillary line.
- V8: Tip of the scapula.
- V9: Paraspinal region.
ST elevation in V7–V9 confirms posterior MI, often accompanied by tall R waves and ST depression in V1–V3.
These extended leads are crucial in patients with persistent symptoms and inconclusive standard ECGs.
How Technology Is Changing Leads on ECG Interpretation
Modern advancements are transforming how we acquire and interpret leads on ecg, making diagnostics faster and more accessible.
Portable ECG Devices and Smart Wearables
Devices like the Apple Watch, KardiaMobile, and AliveCor offer single-lead ECGs that detect atrial fibrillation and other arrhythmias.
- They use modified lead I configuration.
- Limited compared to 12-lead but valuable for screening.
- Integration with smartphone apps allows real-time sharing with physicians.
However, they cannot replace full 12-lead ECGs for diagnosing MI or conduction disorders.
AI-Powered ECG Analysis
Artificial intelligence is being used to interpret leads on ecg with high accuracy. Algorithms can detect subtle patterns missed by humans.
- AI can predict undiagnosed left ventricular dysfunction from a normal-looking ECG.
- Machine learning models classify arrhythmias better than traditional methods.
- Some systems alert clinicians to possible STEMI within seconds of recording.
Companies like Eko and Bay Labs are integrating AI into clinical workflows. Learn more at FDA on AI in ECG.
What do leads on ecg represent?
Leads on ecg represent different electrical perspectives of the heart’s activity, captured by electrodes placed on the limbs and chest. Each lead shows how the electrical impulse travels through the heart from a unique angle, allowing doctors to assess rhythm, conduction, and potential damage.
How many leads are there in a standard ECG?
A standard ECG has 12 leads: six limb leads (I, II, III, aVR, aVL, aVF) and six precordial leads (V1 to V6). These provide a comprehensive view of the heart’s electrical activity in both frontal and horizontal planes.
Can lead misplacement affect ECG results?
Yes, lead misplacement can significantly alter ECG interpretation. For example, placing V1 too high can mimic Brugada syndrome, and arm lead reversal can resemble dextrocardia. Accurate placement is essential for reliable diagnosis.
Why are right-sided and posterior leads used?
Right-sided (V4R–V6R) and posterior (V7–V9) leads are used to detect infarctions in areas not well visualized by standard leads. Right-sided leads help diagnose right ventricular MI, while posterior leads identify posterior wall MI, which may otherwise be missed.
Can wearable devices replace 12-lead ECGs?
No, wearable devices cannot fully replace 12-lead ECGs. While useful for detecting arrhythmias like AFib, they lack the comprehensive spatial resolution needed to diagnose myocardial infarction, axis deviation, or chamber enlargement.
Understanding leads on ecg is fundamental to accurate cardiac diagnosis. From proper electrode placement to interpreting ST changes and avoiding common pitfalls, each aspect plays a vital role in patient care. As technology evolves, the future of ECG interpretation promises even greater precision and accessibility. Whether you’re a medical student, nurse, or physician, mastering the 12 leads is a skill that saves lives.
Further Reading: